Danilo Cimadomo, Laura Rienzi, Alessandro Conforti, Eric Forman, Stefano Canosa, Federica Innocenti, Maurizio Poli, Jenna Hynes, Laura Gemmell, Alberto Vaiarelli, Carlo Alviggi, Filippo Maria Ubaldi, and Antonio Capalbo
ABSTRACT
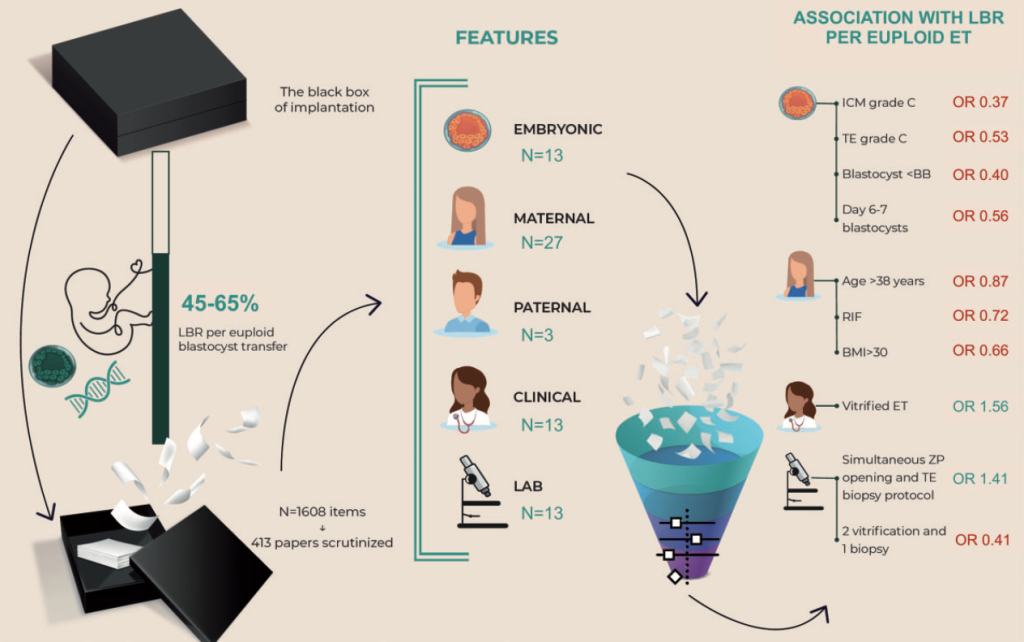
BACKGROUND: A normal chromosomal constitution defined through PGT-A assessing all chromosomes on trophectoderm (TE) biop- sies represents the strongest predictor of embryo implantation. Yet, its positive predictive value is not higher than 50–60%. This gap of knowledge on the causes of euploid blastocysts’ reproductive failure is known as ‘the black box of implantation’.
OBJECTIVE AND RATIONALE: Several embryonic, maternal, paternal, clinical, and IVF laboratory features were scrutinized for their putative association with reproductive success or implantation failure of euploid blastocysts.
SEARCH METHODS: A systematic bibliographical search was conducted without temporal limits up to August 2021. The keywords were ‘(blastocyst OR day5 embryo OR day6 embryo OR day7 embryo) AND (euploid OR chromosomally normal OR preimplantation ge- netic testing) AND (implantation OR implantation failure OR miscarriage OR abortion OR live birth OR biochemical pregnancy OR re- current implantation failure)’. Overall, 1608 items were identified and screened. We included all prospective or retrospective clinical studies and randomized-controlled-trials (RCTs) that assessed any feature associated with live-birth rates (LBR) and/or miscarriage rates (MR) among non-mosaic euploid blastocyst transfer after TE biopsy and PGT-A. In total, 41 reviews and 372 papers were se- lected, clustered according to a common focus, and thoroughly reviewed. The PRISMA guideline was followed, the PICO model was adopted, and ROBINS-I and ROB 2.0 scoring were used to assess putative bias. Bias across studies regarding the LBR was also assessed using visual inspection of funnel plots and the trim and fill method. Categorical data were combined with a pooled-OR. The random effect model was used to conduct the meta-analysis. Between-study heterogeneity was addressed using I . Whenever not suitable for the meta-analysis, the included studies were simply described for their results. The study protocol was registered at http://www. crd.york.ac.uk/PROSPERO/ (registration number CRD42021275329).
OUTCOMES: We included 372 original papers (335 retrospective studies, 30 prospective studies and 7 RCTs) and 41 reviews. However, most of the studies were retrospective, or characterized by small sample sizes, thus prone to bias, which reduces the quality of the evidence to low or very low. Reduced inner cell mass (7 studies, OR: 0.37, 95% CI: 0.27–0.52, I2 1⁄4 53%), or TE quality (9 studies, OR: 0.53, 95% CI: 0.43–0.67, I2 1⁄4 70%), overall blastocyst quality worse than Gardner’s BB-grade (8 studies, OR: 0.40, 95% CI: 0.24–0.67, I2 1⁄4 83%), developmental delay (18 studies, OR: 0.56, 95% CI: 0.49–0.63, I2 1⁄4 47%), and (by qualitative analysis) some morphodynamic abnormali- ties pinpointed through time-lapse microscopy (abnormal cleavage patterns, spontaneous blastocyst collapse, longer time of morula formation I, time of blastulation (tB), and duration of blastulation) were all associated with poorer reproductive outcomes. Slightly lower LBR, even in the context of PGT-A, was reported among women 38 years (7 studies, OR: 0.87, 95% CI: 0.75–1.00, I2 1⁄4 31%), while obesity was associated with both lower LBR (2 studies, OR: 0.66, 95% CI: 0.55–0.79, I2 1⁄4 0%) and higher MR (2 studies, OR: 1.8, 95% CI: 1.08–2.99, I2 1⁄4 52%). The experience of previous repeated implantation failures (RIF) was also associated with lower LBR (3 studies, OR: 0.72, 95% CI: 0.55–0.93, I2 1⁄4 0%). By qualitative analysis, among hormonal assessments, only abnormal progesterone levels prior to transfer were associated with LBR and MR after PGT-A. Among the clinical protocols used, vitrified-warmed embryo transfer was more effective than fresh transfer (2 studies, OR: 1.56, 95% CI: 1.05–2.33, I2 1⁄4 23%) after PGT-A. Lastly, multiple vitrification-warming cycles (2 studies, OR: 0.41, 95% CI: 0.22–0.77, I2 1⁄4 50%) or (by qualitative analysis) a high number of cells biopsied may slightly reduce the LBR, while simultaneous zona-pellucida opening and TE biopsy allowed better results than the Day 3 hatching-based protocol (3 studies, OR: 1.41, 95% CI: 1.18–1.69, I2 1⁄4 0%).
WIDER IMPLICATIONS: Embryo selection aims at shortening the time-to-pregnancy, while minimizing the reproductive risks. Knowing which features are associated with the reproductive competence of euploid blastocysts is therefore critical to define, imple- ment, and validate safer and more efficient clinical workflows. Future research should be directed towards: (i) systematic investiga- tions of the mechanisms involved in reproductive aging beyond de novo chromosomal abnormalities, and how lifestyle and nutrition may accelerate or exacerbate their consequences; (ii) improved evaluation of the uterine and blastocyst-endometrial dialogue, both of which represent black boxes themselves; (iii) standardization/automation of embryo assessment and IVF protocols; (iv) additional invasive or preferably non-invasive tools for embryo selection. Only by filling these gaps we may finally crack the riddle behind ‘the black box of implantation’.